Artificial intelligence is a tool to help doctors, not replace them: Dr. Siegel
Fox News contributor Dr. Marc Siegel weighs in on how artificial intelligence can change the patient-doctor relationship on ‘America’s Newsroom.’
It’s been shown to detect cancer, pinpoint cavities and answer medical questions — and now, artificial intelligence may help fertility doctors select the ideal embryo for in-vitro fertilization (IVF).
With one in every five U.S. adult married women unable to get pregnant after a year of trying, per the Centers for Disease Control and Prevention (CDC), many turn to IVF for help. The fertility treatment is responsible for between 1% and 2% of all births in the country.
The process, however, is not guaranteed — and it’s expensive, averaging more than $12,000 per session, according to the American Society of Reproductive Medicine. And most women require more than one attempt.
AIVF, a reproductive technology company based in Tel Aviv, Israel, aims to improve the odds.
Its AI-powered embryo evaluation software, called EMA, is designed to process vast amounts of data — beyond what the human eye can detect — to simplify the embryo selection process.

AIVF, a reproductive tech company in Tel Aviv, Israel, offers an AI-powered embryo evaluation software, EMA, to simplify the embryo selection process. Shown here are AIVF team members. (AIVF)
"IVF is one of the most important medical developments in the last 50 years, but it’s not good enough," Daniella Gilboa, an embryologist who is co-founder and CEO of AIVF, told Fox News Digital.
"Success rates are about 23% to 25% across all age groups, which means only one in five result in pregnancy."
In the U.S., only 20% of the demand for IVF can be met by existing clinics, said the CEO of AIVF, which is based in Israel.
One of the biggest challenges is that IVF clinics can’t keep up with the growing demand, Gilboa said.
"More women are freezing their eggs so they can delay childbirth and focus on their careers, which means demand for IVF is growing — but supply is limited," she said.
CHEMICALS IN WATER AND HOUSEHOLD OBJECTS COULD REDUCE CHANCES OF PREGNANCY, LIVE BIRTHS: NEW STUDY
"In the U.S., only 20% of the need is served, which means 80% of those women are giving up on the dream of having a child."
One of the most crucial decision points during the IVF process is embryo selection, Gilboa explained.

"IVF is one of the most important medical developments in the last 50 years, but it’s not good enough," Daniella Gilboa, an embryologist who is the co-founder and CEO of AIVF (pictured here), told Fox News Digital. (AIVF)
Traditionally, human clinicians have been tasked with making that choice on their own.
"Imagine if you’re an embryologist, looking at multiple embryos in a hectic lab environment, and you have to decide which one has the best potential to become a baby," she said.
"You might have eight, 10 or 12 embryos that all look the same — and you have to make that crucial decision, sometimes by yourself. It’s basically you and the embryos under the microscope."
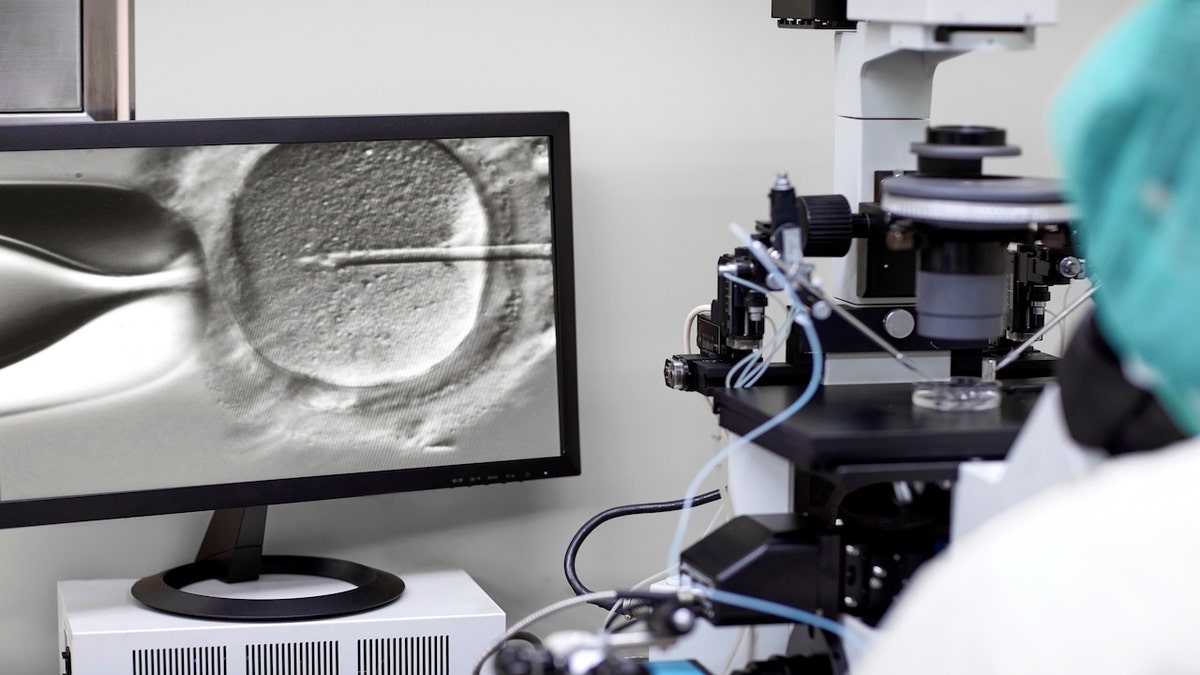
Traditionally, human clinicians have been tasked with making IVF embryo selections on their own. (iStock)
With AIVF’s EMA software, an AI model helps the clinician by evaluating embryos and applying its advanced algorithm to determine the best candidates for a successful pregnancy.
"The AI has been trained to detect embryonic features that correlate to different outcomes — like genetic abnormalities, implantation or gender — that can’t be seen with the human eye," Gilboa said.
Each embryo gets a numeric score. The clinician can then make the final decision.
With one in every five U.S. adult married women unable to get pregnant after one year of trying, many turn to the IVF process for help. (iStock)
Without AI, said Gilboa, clinicians would have to rely on the appearance of the embryo to determine its quality — "but that's based on subjective human analysis that doesn't really quantify the actual chances of getting pregnant," she added.
"At the end of the day, the human makes the decision, not the AI."
"The AI allows the physician to reduce uncertainties and produce clear, accurate information."
The AI is also much faster, evaluating embryos in a fraction of the time that it takes a human, she said — which means clinics can see more patients and meet more demand.
AI MAY HAVE AN ‘EYE’ ON GROWING BABIES: COULD PREDICT PREMATURE BIRTH AS EARLY AS 31 WEEKS
EMA’s AI software was trained on vast numbers of time-lapse videos of embryos in development, learning which ones had positive outcomes and which were not viable.

The AI tech could potentially reduce the cost for the patient, because it could result in viable pregnancies in fewer sessions, said the CEO of AIVF. (iStock)
"You need a huge amount of data," Gilboa said. "It was a long process, with many durations, to build a model that was good enough to start using."
‘Very welcomed’
Dr. Shahin Ghadir, a double board-certified infertility expert and Trimly fertility coach in California, said AI technology like AIVF’s could be "helpful and useful." (Trimly is an online health care advisory service.)
"The field of reproductive medicine and fertility has had major limitations in growth because of the lack of manpower and expertise available to work in this industry," Ghadir told Fox News Digital.
"Since embryologists are very limited and hard to train, this technology would be very welcomed."
OZEMPIC, WEGOVY AND PREGNANCY RISK: WHAT YOU NEED TO KNOW ABOUT THE ISSUE
He added, "I think embryologists are still needed in the laboratory, but combining their expertise with the use of artificial intelligence may be extremely helpful."
A tool, not a replacement
Although EMA helps to optimize and expedite the embryo selection process, Gilboa pointed out that it is not intended to replace doctors.
"At the end of the day, the human makes the decision, not the AI," she said. "It’s just a tool that helps the clinician evaluate the embryos, consult with the patient and provide better IVF care."
"It’s not ‘humans versus AI' — it’s ‘humans with AI.'"
With AIVF’s EMA software, an AI model (not pictured) helps the clinician by evaluating embryos and applying its advanced algorithm to determine the best candidates for a successful pregnancy. (iStock)
While Ghadir supports evaluating the capabilities of artificial intelligence, he emphasized that it must be "scrutinized under significant criteria" before it’s rolled out.
"Some of the risks and limitations of artificial intelligence in an IVF setting and laboratory include errors in grading of embryos that could potentially affect outcomes," he said.
"Through advanced AI, patients who dream about having a baby can be part of the IVF process with full laboratory transparency."
"The recommendation for using AI in this environment would be to do a side-by-side expertise evaluation for a period of time — until there is complete confidence that the AI is as good as the expert evaluations."
The idea of using AI in embryo selection may also involve some ethical considerations, which can impact the personal decisions of individual patients and families.
Looking ahead
AIVF’s technology is right now in use in Europe, Southeast Asia and South America, and is expected to be available in the U.S. "very soon," Gilboa said.
Among the clinics that have purchased the software and are using it, the feedback has been positive.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
"We have reports that clinics have seen a 30% increase in IVF success rates," Gilboa said.
The tech could also potentially reduce the cost to the patient, she added, because it could result in viable pregnancies in fewer sessions.
CLICK HERE TO GET THE FOX NEWS APP
"With traditional IVF, it takes an average of three to five treatments to achieve pregnancy — but with AIVF, the average is 1.6 treatments," she said.
Added Gilboa, "Through advanced AI, patients who dream about having a baby can be part of the IVF process with full laboratory transparency."





















