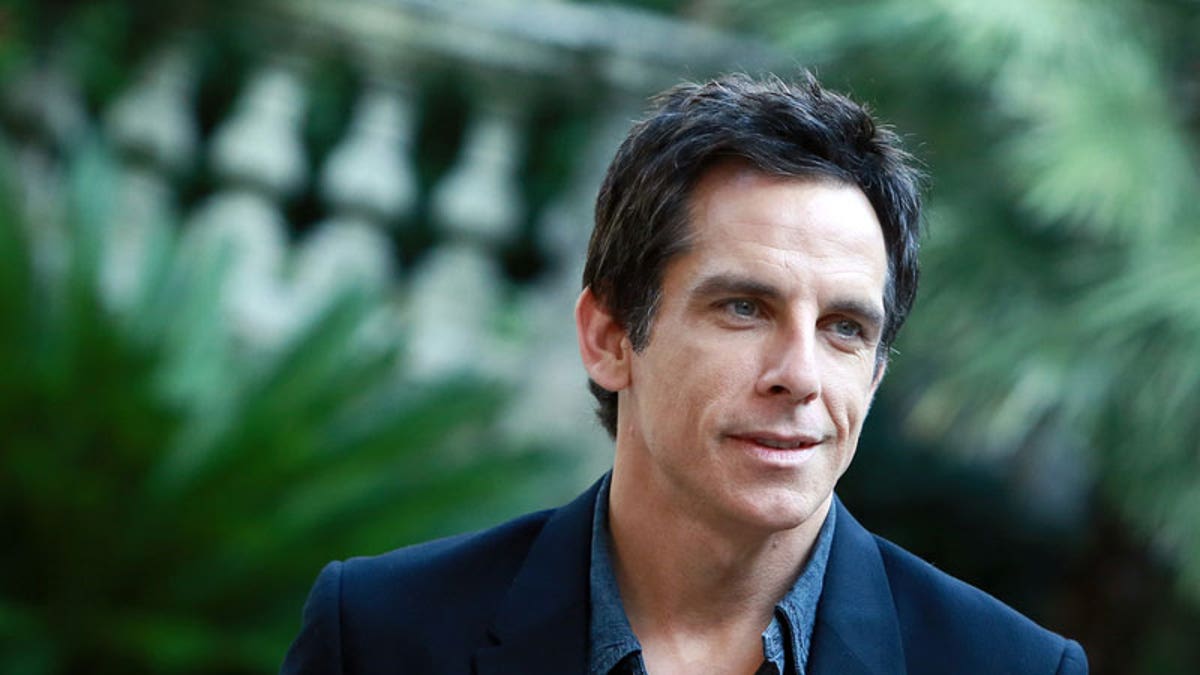
Ben Stiller in Rome in 2013. (Lucky Team Studio / Shutterstock.com)
Actor Ben Stiller is crediting a prostate cancer screening test for saving his life, revealing today that he was diagnosed and treated for prostate cancer two years ago. But should all men get this screening test?
In an interview today (Oct. 4) on The Howard Stern Show, Stiller revealed for the first time that he was diagnosed with prostate cancer at age 48. The actor, who is now 50, said doctors detected the cancer because Stiller had undergone a prostate-specific antigen test, or PSA test, which looks for levels of the protein PSA in the blood. Abnormally high levels of PSA in the blood can mean that a man has prostate cancer, but not always. In Stiller's case, a follow-up MRI and biopsy showed he had prostate cancer.
"This thing saved my life," Stiller said of the PSA test.
The PSA test is the main test used to screen for prostate cancer, but it is controversial. In 2012, the U.S. Preventive Services Task Force, or USPSTF (an expert panel that advises the federal government) recommended that men not undergo routine screening for prostate cancer with the PSA test, no matter their age.
The American Cancer Society recommends that men have a discussion with their doctor about whether to start PSA screening at age 50 if they are at average risk for prostate cancer, and at age 40 to 45 if they have a family history of prostate cancer.
The main issue with prostate cancer screening is that, although the PSA test can help detect prostate cancer early, it's not clear if the test's benefits outweigh its risks in the long run for most men.
One problem with the PSA test is that it often suggests that men have prostate cancer when they do not have cancer, according to the USPSTF. About 75 percent of men with abnormally high levels of PSA do not have cancer. These so-called false positive results can lead to anxiety and unnecessary follow-up tests, the USPSTF says.
The PSA test doesn't always detect cancer, either — about 20 percent of men with prostate cancer have normal PSA levels, so the test may give these men a false sense of security, according to Harvard Medical School.
What's more, even when true prostate cancer is detected, doctors cannot tell for sure whether the prostate cancer poses an actual threat to a man's health.
In many cases, prostate cancer does not grow or cause symptoms, or it grows so slowly that it would never have caused problems in a patient's lifetime, according to the USPSTF.
"Because of an elevated PSA level, some men may be diagnosed with a prostate cancer that they would have never even known about at all. It would never have led to their death, or even caused any symptoms," the American Cancer Society says.
This means that some men with prostate cancer get treatment that they don't need. And the treatments for prostate cancer, such as surgery and radiation, are not benign. They can lead to erectile dysfunction, urinary incontinence and problems with bowel control.
More From LiveScience
Indeed, Stiller told Stern about some of the side effects of his treatment, saying that sex was different for him after the surgery. "It takes time to come back," Stiller told Stern. "It changes the experience of what an orgasm feels like. It's great; it just feels different."
Overall, it's not clear if detecting prostate cancer early reduces a man's risk of dying from the disease. A 2012 study of 76,000 men found that those who underwent yearly screening for prostate cancer were just as likely to die from the disease over a 13-year period as those who underwent screening only if their doctor recommended it.
Many experts believe a practice known as active surveillance could reduce unnecessary treatment of the disease. Under active surveillance, patients diagnosed with low-risk prostate cancer receive regular follow-up testing and are treated only if their cancer becomes more aggressive.
Still, a recent study found that men with prostate cancer were just as likely to die from the disease over a 10-year period regardless of whether they received active surveillance, surgery or radiation as treatment.
But the study also found that men who underwent active surveillance after their diagnosis were more likely to eventually have their cancer progress and spread to other parts of their body than men who received surgery or radiation shortly after their diagnosis. And about half of the men who started out with active surveillance ended up needing treatment with surgery or radiation.
The researchers on that study, which was published Sept. 14 in The New England Journal of Medicine, concluded that they will need to keep following the study participants for a longer period of time to draw further conclusions. They hope that continued follow-up will tell them whether the patients who received active surveillance will eventually show a difference in their death rate, compared with the men in the other groups.
"Men with newly diagnosed, localized prostate cancer need to consider the critical trade-off between the short-term and long-term effects of radical treatments on urinary, bowel and sexual function and the higher risks of disease progression with active monitoring, as well as the effects of each of these options on quality of life," the researchers said.
Original article on Live Science.