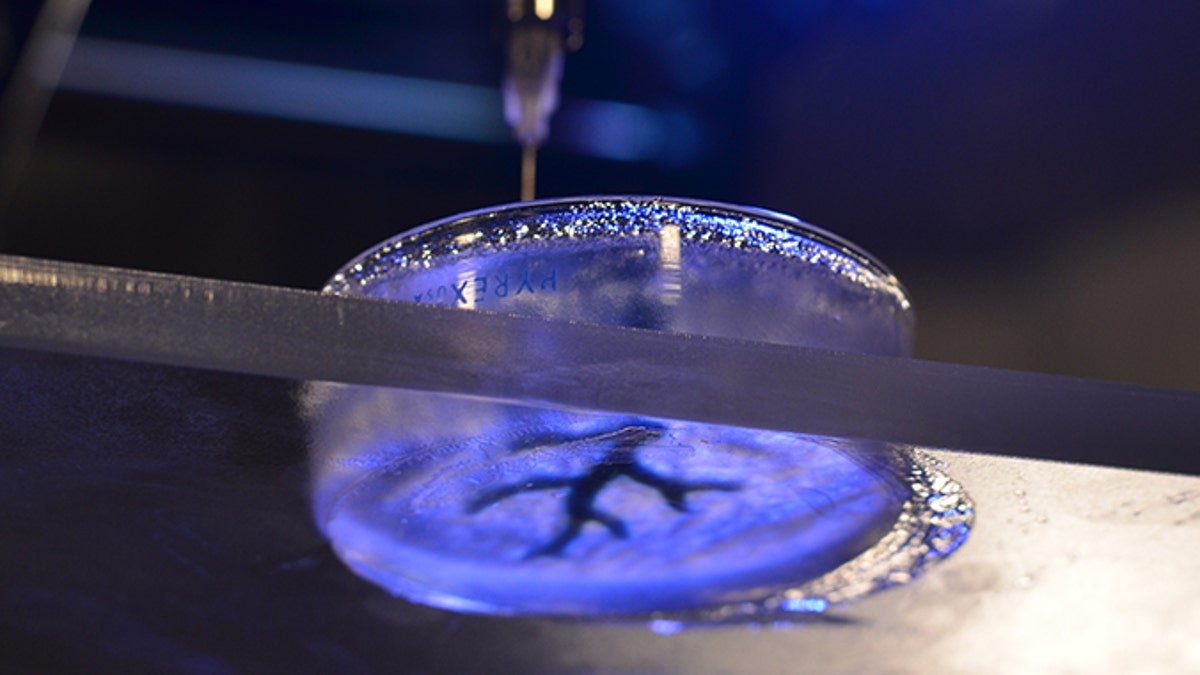
The technique involves filling a petri dish with a semiliquid mixture, dropping a syringe inside and 3-D printing soft material like collagen and fibrin, which are similar to biological components. (Carnegie Mellon University College of Engineering)
While 3-D printing has been around for the past few decades, so far the majority of doctors use the technology for replicating custom human models with hard material to facilitate surgical planning. But in labs across the world, scientists are working on advancing the method to print soft materials for research and, one day, the design of custom organs for patients who need transplants.
Adam Fienberg, an associate professor of bioengineering and materials science at Carnegie Mellon University, is one of those scientists who are pushing boundaries in 3-D printing. In the Oct. 23 issue of the journal Science Advances, Feinberg’s team published details on a new method that involves 3-D printing collagen gel within another gel that helps support it. For their study, they used an open-source 3-D printer to prove the method works, and show that the technique helped them 3-D print coronary arteries and embryonic hearts.
“We were inspired by Jell-O,” Feinberg, the lead author of the study, told FoxNews.com of the technique. “If you’ve seen fruit hanging inside Jell-O, you can appreciate that Jell-O holds things inside it. We wanted to come up with something like a Jell-O mold where we could print something inside.”
Although the idea for printing soft materials has always been at the forefront of scientists’ minds, coming up with an effective means for executing the task has proven challenging. That’s because— unlike 3-D printing hard materials that maintain their shape when touched— 3-D printing soft materials involves putting one layer down and another layer on top while ensuring the bottom portion, which is malleable, remains perfectly positioned.
Feinberg’s team found a way around that obstacle by using what they call a “support bath” made of gelatin slurry, which is a semiliquid mixture. This slurry contains micro-gel particles that collectively act like wet sand in their ability to conform to objects they come into contact with. In other words, the solution behaves like a liquid if you move it but like a solid if you don’t.
Researchers filled a petri dish with the support bath, dropped a syringe inside and began 3-D printing soft material like collagen and fibrin, which are similar to biological components.
“What we were able to do is create a lot of proof of concept, basically showing we could create things like scaffolds for blood vessels,” Feinberg said. “That’s important because those are the vessels that are blocked during heart attack, and right now, there’s no good way to fix that.”
Heart disease is the leading killer in the world and is responsible for one in four deaths in the United States every year, according to the Centers for Disease Control and Prevention (CDC). Primary treatment options for the disease include medications, and surgical and non-surgical operations. In severe cases, patients may require a heart transplant, which depends on the availability of a suitable donor organ.
With their new method, Feinberg’s team showed a similar proof of concept for the embryonic heart. He said they are pursuing that idea to learn how to grow part of a human heart to repair damage to the organ— a feat he expects scientists to achieve within the next decade, but one that could not be applied in a clinical setting without approval from the Food and Drug Administration (FDA).
“There’s a lot of moving pieces,” Feinberg said. “What we’re building are the tools to build tissues, but we also need the right cells to put in there. Stem cell biology needs to build the right cells from which we can build large human heart cells to put into scaffolds.”
Christine Mummery, professor of developmental biology and the chair of the department of anatomy and embryology at Leiden University Medical Center in The Netherlands, is studying how to turn stem cells into cardiac muscle cells. Her research could one day help enable scientists to test how certain drugs perform in people with genetic disorders. But so far, her team has used only 2-D printing, which keeps cells in an immature state, making modeling realistic heart disease difficult.
“We believe if we put them in 3-D and allow them to be in a sort of vacuum and sort of stretch them, then they may become more like adult cells,” Mummery, who was not involved in Feinberg’s current research, told FoxNews.com. “This [difference] is what Adam [Feinberg] could maybe achieve.”
Jordan Miller, an assistant professor of bioengineering who specializes in bioprinting at Rice University, who was also not involved in the current study, called Feinberg’s method “exciting.”
“They really could do things that you can’t do by melt excursion or by inkjet programs and stereolithography,” which are three other methods for 3-D printing material, Miller told FoxNews.com. “Not only are they making structures that are difficult or impossible to make, and that those methods can’t, but they’re doing it with materials that haven’t historically worked with those methods too well.”
“This work takes a very important step in demonstrating the ability to fabricate some of the complex architectures that are found in the body,” he added, “and we’ll be really excited to see if these structures can have the same mechanical resilience and integrity and function of the tissues that they are structured after.”
Feinberg expects that within the next two years, his team’s support bath method could be applied for the creation of human heart muscle tissue that could be tested against experimental drugs. The standard for FDA approval today first involves screening drugs in rodents, but how rodents react to drugs aren’t predictive of how they’ll act in humans.
“The number-one reason [drugs] fail in studies is because of toxicity to the heart and liver, so if you can screen that out before clinical trials, you can find out much faster if there will be side effects and if it will be viable as a therapy in humans,” he said.
Feinberg pointed out that the strategy could be used to help scientists identify relationships between certain coronary characteristics and adverse drug reactions in exceptional groups as well. For instance, some types of chemotherapy are extremely toxic to the point that the patient needs a heart transplant. While this effect happens in only a small percentage of the population, if doctors can identify groups like these, they can improve their treatment strategies.
“In terms of whether we’ll ever make a whole heart for transplantation, that’s a long way off,” said Mummery, the stem cell scientist from Leiden University. “But with science, it’s not really the end result; it’s what you develop along the way and what you learn.”