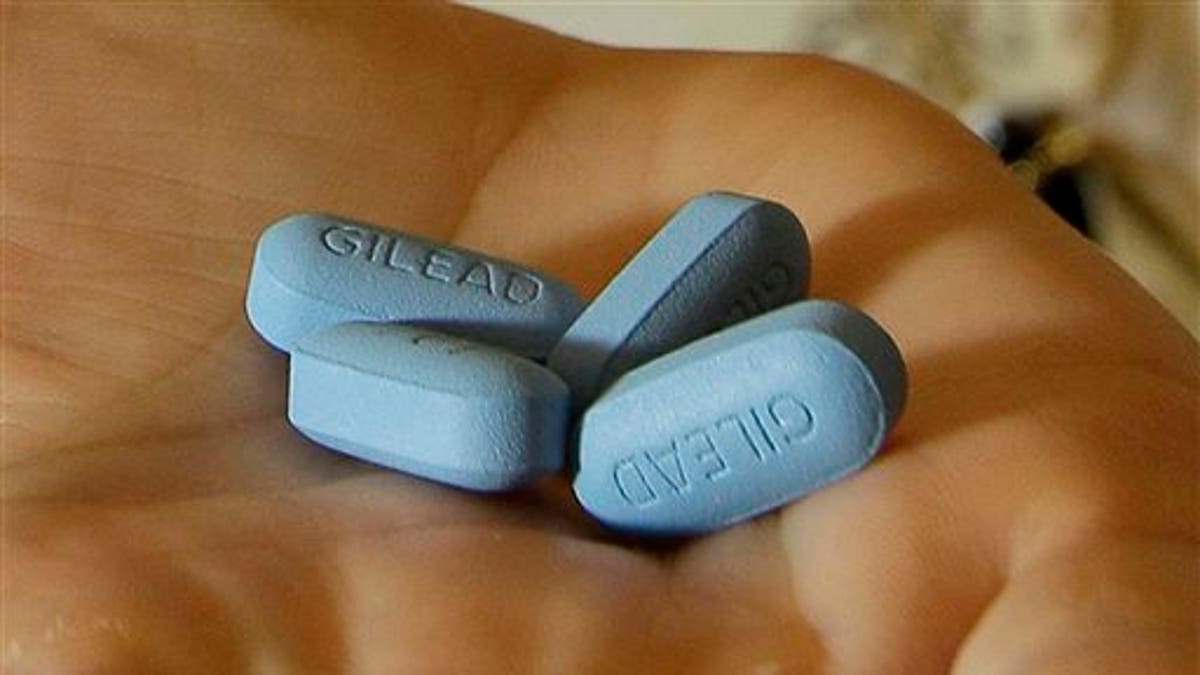
In this Thursday, May 10, 2012 file photo, a doctor holds Truvada pills at her office in San Francisco. (AP Photo/Jeff Chiu)
Gay and bisexual men who take a Truvada pill daily to prevent infection with HIV did better than researchers expected at sticking to their medication schedule, according to a new report.
But overall, doctors aren't prescribing the drug to enough of the men who could use it, the study found.
Out of more than 1,000 gay and bisexual men surveyed, only 83, or fewer than one in 10, reported that they use HIV pre-exposure prophylaxis (PrEP).
But 42 percent of those who do use it said they had not skipped a single dose in the previous 90 days, and only 6 percent had skipped more than two doses per week, the investigators reported at the annual meeting of the Society of Behavioral Medicine in Washington, DC.
The lesson for care providers is that men are willing and able to take a daily pill, so it is important to talk to those who could benefit and increase prescription rates, study leader Jeffrey Parsons, a professor of psychology at Hunter College, City University of New York, told Reuters Health by email.
"The majority of gay men who are . . . good candidates for PrEP are not on the medication, and many haven't spoken to their medical providers about PrEP. We need to get conversations going, and in general promote more open dialogue between doctors and patients regarding sexual health," Parsons said.
The U.S. Centers for Disease Control has guidelines to help healthcare providers determine who is an appropriate candidate for PrEP with safer sex practices and Truvada, a pill made by Gilead that contains the antiviral drugs emtricitabine and tenofovir.
The findings are from One Thousand Strong, a three-year observational study of a U.S. national sample of gay and bisexual men ages 18 to 80 that is now underway.
The diversity of the sample is what lends this study its strength, said Dr. Kathy Goggin of Children's Mercy Hospitals and Clinics and the University of Missouri - Kansas City Schools of Medicine and Pharmacy, who is not involved in the research.
"Because of the uniqueness of this cohort - participants reside in rural and urban settings across the county - this study provides a truly novel snapshot of what is really happening in the real world right now, and it's very encouraging in terms of adherence. Uptake is another story," Goggin says.
The lingering stigma of men who have sex with men may explain much of the low uptake, both researchers say.
"I think we have a way to go on getting the message out to men and providers that PrEP can really help a lot more people than are currently on it and that stigma and negative associations with PrEP still persist," Goggin says.