Fox News Flash top headlines for June 1
Fox News Flash top headlines are here. Check out what's clicking on Foxnews.com.
Scientists are trying to better understand why monkeypox is spreading rapidly across the world in regions that do not typically harbor the disease since the United Kingdom confirmed its first case of monkeypox in early May.
"We've never really seen this type of observation from monkeypox before, so this is particularly concerning," said Andrea McCollum, an epidemiologist who heads the poxvirus team at the Centers for Disease Control and Prevention (CDC).

In this Centers for Disease Control and Prevention handout graphic, symptoms of one of the first known cases of the monkeypox virus are shown on a patient’s hand. (Courtesy of CDC/Getty Images)
Over 550 confirmed cases of monkeypox in 30 countries have been detected globally, including approximately 18 in the United States, according to the World Health Organization (WHO) and the CDC.
"We're seeing cases all appearing in a relatively short period of time. We're seeing that in a few days, in a couple of weeks, we're seeing over 500 cases. This is different. This has not been seen before," said Rosamund Lewis, WHO’s technical lead for monkeypox.
The CDC notes monkeypox belongs to the same genus of virus as smallpox, but after smallpox was eradicated by worldwide vaccination in 1980, waning immunity against monkeypox may have contributed the surge in cases since smallpox vaccination is no longer recommended, according to Nature.
WHO: MONKEYPOX NOT EXPECTED TO BECOME PANDEMIC, MUCH REMAINS UNKNOWN
Africa usually has a few thousand cases in an average year, mostly in the western and central parts of the region, but just in the past week the cases outside Africa have exceeded the total number detected outside the continent since 1970, when the first human case was detected.
But even though scientists are worried about the rapid spread of monkeypox, it’s no coronavirus, according to Nature.
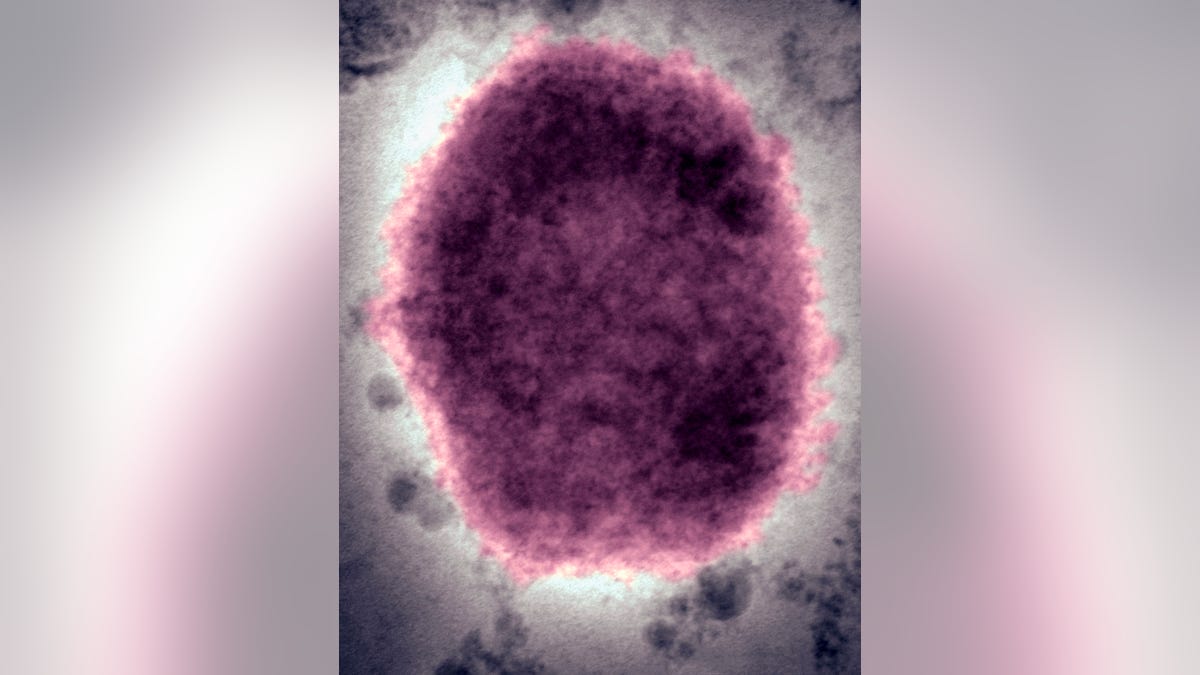
A negative stain electron micrograph reveals a "M" Mulberry Type monkeypox virus virion in human vesicular fluid. (BSIP/UIG Via Getty Images)
Monkeypox is not as infectious as SARS-CoV-2, the virus responsible for the COVID-19 pandemic, because it does not transmit from person to person as easily and because we have vaccines to prevent it, said Jay Hooper, a virologist at the United States Army Medical Research Institute of Infectious Diseases in Fort Detrick, Maryland.
SARS-CoV-2 spreads through tiny droplets in the air called aerosols, but scientists believe monkeypox spreads primarily through close contact with bodily fluids, so a person infected with monkeypox will infect a lot fewer close contacts than someone infected with the coronavirus, Hooper added.
Research from sequencing viral genomes from people infected with monkeypox in Belgium, France, Germany, Portugal and the United States suggests the monkeypox strain resembles the much less lethal strain found in West Africa, which has a death rate of less than 1% in rural populations. In comparison, the much more virulent strain in Central Africa has a fatality rate up to 10%, according to Nature.
MONKEYPOX AND ENDEMIC DISEASES BECOMING MORE PERSISTEN, WHO SAYS
These sequences are most similar to the cluster of monkeypox cases that cropped up outside outside Africa in 2018 and 2019 and were linked to travel in West Africa.
So the simplest explanation is the person who had the first non-African case of the year became infected through either animal contact or close contact with someone already infected with the virus while traveling to a similar region in Africa, says Bernie Moss, a virologist at the National Institute of Allergy and Infectious Diseases.
Researchers hope to discover if the rapid rise in cases are from a viral mutation that allows monkeypox to transmit more easily, says Dr. Raina MacIntyre, an epidemiologist specializing in infectious diseases at the University of New South Wales in Sydney, Australia.
But unlike SARS-CoV-2, which is an RNA virus that is adept at evading immunity from vaccines or prior infection, monkeypox is a DNA virus, which are known to be better at repairing mutations than RNA viruses. This means the monkeypox virus is less likely to suddenly mutate and make person-person transmission easier, MacIntyre added.
But it’s still "deeply concerning" monkeypox cases are rising in people with no connection to one another, McCollum said.
Scientists are also trying to discover why the case clusters include mostly men ages 20-50 years old, many who have sex with men (MSM), but MacIntyre says it could be coincidental that the virus was introduced into a MSM community and continued to spread as it is not known to be a sexually transmitted infection.
United Kingdom Health Security Agency, however, recommends symptomatic monkeypox patients should abstain from sexual activity while lesions are present even though there is no known evidence of the virus in genital excretions. In addition, they recommend use of condoms for eight weeks after infection.

In this Centers for Disease Control and Prevention handout graphic, symptoms of one of the first known cases of the monkeypox virus are shown on a patient’s hand. (CDC/Getty Images)
Although the CDC notes there is no specific treatment for monkeypox, several antivirals may prove to be beneficial.
In addition, the United States has a stockpile of millions of smallpox vaccines, two of which are approved and are generally effective also against monkeypox.
The CDC’s Advisory Committee on Immunization Practices recently published recommendations to limit the use of the smallpox vaccine known as Jynneos to healthcare workers and laboratory personnel who work closely with the virus.
McCollum noted these therapies will not be deployed on a large scale, but instead close contacts of those infected with monkeypox will be vaccinated in a method called "ring vaccination."
CLICK HERE TO GET THE FOX NEWS APP
"The first part is to identify those who are infected and to isolate them and make sure that they get the care they need," said Dr. Raj Panjabi, who leads the White House's monkeypox response.
"The second part is to ensure we vaccinate those who've been exposed to the infected individuals. If we do that again and again – and that's our approach at the White House and across the government – then we have a better chance of ending this outbreak."
