Tree service hangs giant US flag, 'thank you' sign at hospitals during coronavirus crisis
A Connecticut tree service is showing their appreciation for local health care workers in a big way.
Get all the latest news on coronavirus and more delivered daily to your inbox. Sign up here.
As New York continues to bear the nation’s brunt of the coronavirus pandemic, the city’s Veteran’s Affairs (VA) hospitals have opened up their beds to civilians for the first time in its 66-year history.
“This has never been done before, so we’re making history,” Martina Parauda, director of the New York VA, Harbor Health System (HHS) told Fox News. “Our hospital is proud to be part of the community here and assist New York City in such a time of need.”
The fundamental decision was made on March 29 as part of the Department’s “Fourth Mission,” as concerns escalated that the novel coronavirus could overwhelm the state’s health care system.
The Department of Veteran Affairs thus announced it was assisting the city with its COVID-19 response by opening 50 beds – 35 acute, 15 ICU.
According to Parauda, FEMA made the request after New York State asked for federal assistance, and the VA “made its decision after determining this action would not negatively impact veteran care.”
CLICK HERE FOR COMPLETE CORONAVIRUS COVERAGE
Jodie Jackson, associate director of the VA in New York, explained that the non-veteran beds are located at their Manhattan and Brooklyn VA medical centers.
At this stage, those VA locations are treating a combination of “positive, presumptive, and non-coronavirus patients,” Jackson noted. As of this week, the New York VA system has treated more than 80 civilian patients.
However, officials emphasized that the VA – which has long come under scrutiny over its health care capacity for the growing number of former service members – has additional bed capacity available for the city, but that its priority is to ensure bed space for veterans as they discharge and accept new patients.
“We have a specialized clinical triage team led by one of our doctors, who works with city and private hospitals to determine which patients have the greatest need,” Jackson noted. “For example, a hospital we’re working with had a catastrophic failure of their oxygen system, and we were able to immediately accept some of their patients – saving their lives.”
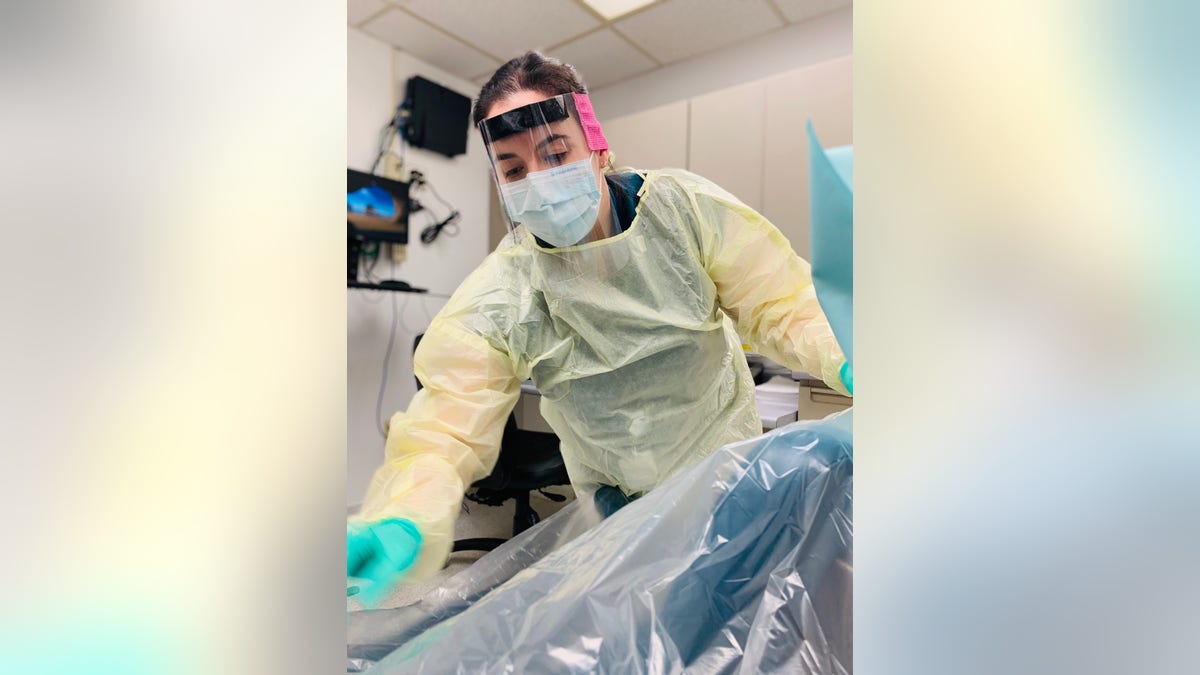
Dr. Sarah Schuback, a dentist with Dental Services, VA NY HHS, wears a field shield she helped construct while preparing an exam room for patients. (Courtesy VA NY HHS)
ON CORONAVIRUS, CHINA AND WHO SHOW THEY’VE LEARNED LITTLE AFTER 2003 SARS OUTBREAK
Nonetheless, the civilian bed openings are far from the only adaption the VA has been forced to make in recent weeks. Jackson also highlighted that, in conjunction with the CDC guidelines on social distancing, they have requested that patients only show up at the medical centers if it’s an emergency.
“For non-emergencies, we’ve increased our telehealth efforts and leaned on existing systems like secure messaging and teleconferencing with doctors,” she continued. “Veterans are meeting with their providers in virtual care rooms, calling helplines and more.”
Such telecare efforts have not only been extended to health treatment – including an increase in mental health services during this epoch of unprecedented emotional and financial stress – but also to the homeless veteran population.

Tanya Garcia, a patient care team coordinator in the intensive care unit, works the front lines in the battle against COVID-19. Her supervisors describe her as an extremely skilled clinician and manager, loved by her staff for her ability to bring calm in times of chaos. (Courtesy VA NY HHS)
For veterans who are housed in the VA’s HUD/VASH program, or in transitional housing through grant and per-diem or contract housing, social workers use virtual platforms and calls to assess health and safety, provide information, and continue to assist in the housing process.
“The homeless program received a generous donation of 60 cell phones with data plans for vets without phones to stay in touch with their providers,” said Karen Fuller, the Homeless Programs Manager, for the New York VA. “Social workers and nurses are distributing the phones to veterans in need, and continue to stay in touch even when they can’t do in-person visits.”
The housing process continues though some of the protocols have had to adapt to a more virtual approach, Fuller underscored. For example, housing applications are now sent electronically rather than dropped off in person at the housing authority.

Jack Berman, a 95-year-old World War II Navy veteran, was briefly hospitalized and released into our housing program. He’d lost his phone while traveling to the hospital, so the social workers provided him with a phone preloaded with care provider phone numbers and telehealth apps. (Courtesy VA NY HHS)
Over the past few weeks, the homeless program team compiled a list of some of our most vulnerable, at-risk veterans living on the streets and shelters and developed an outreach plan to provide on-site health assessment, nursing care, and deliver food and mobile phones they can use to be contacted and access telehealth services.
One such veteran is Sydney Brown, a 70-year-old Vietnam Air Force veteran, who has been working with the HUD/VASH's Assertive Community Treatment Team since 2017. After decades of street and shelter homelessness, Brown has been able to maintain an apartment and live independently with the support of the team’s weekly visits, and residence and family support.
CORONAVIRUS CRISIS: DOZENS OF AMERICANS STRANDED IN TONGA APPEAL FOR HELP TO GET OUT AS CYCLONE HITS
Yet when the ascending coronavirus contagion slammed the city last month, VA workers said that they were unable to contact and assess Brown’s health status, functioning and food access, due to him not having a phone. Thankfully, as a result of the phone donation “from a large telecom company,” nurse practitioner Ellen Flanagan and nurse Ken Brereton traveled to his residence, and with the use of Personal Protective Equipment (PPE), get the phone activated and programmed with team contacts and virtual health apps.
Brown’s “hello” calls are, staffers say, a welcome relief for both parties.

Michael Shepherd, a licensed clinical social worker at VA NY HHS, works with homeless and at risk veterans. Here, he provides a preloaded cell phone to a veteran, enabling him to contact his healthcare providers and access telehealth apps. (Courtesy VA NY HHS)
The U.S. military and veteran communities have, along with much of the country, been hit hard by the deadly pandemic.
On Monday, it was confirmed that a sailor onboard the USS Theodore Roosevelt died from coronavirus, and that at least 585 on the ship have tested positive. At least seven health care workers at five different VA hospitals around the country are also reported to have died from the pathogen, and more than 1,100 have been forced into quarantine.
Moreover, VA top-brass is also warning veterans to avoid traveling to the facilities as the nation’s leaders battle to control the devastating disease, which has already claimed the lives of more than 26,000 Americans.
“We realize the COVID-19 epidemic is a stressful time for our veterans and want to reinforce we’re available – at any time – to respond to veterans during this crisis. In most cases, veterans’ healthcare questions and prescription renewals can be handled without them traveling to the facility,” added Dr. Patrick Malloy, executive chief of staff, of the VA New York.
“Veterans with symptoms like fever, cough, or shortness of breath should immediately contact the facility to speak with a nurse or their provider before visiting. Vets can access online resources and telehealth offerings while practicing social distancing to reduce risk to themselves and others. Veterans concerned about the virus should download the Annie app, which helps monitor symptoms and advises when to contact their VA care team or a nurse triage line.”


